Defeating Prescribing Cascades to Better Help Your Patients
2024-02-15
|Barbara St-Pierre, B.Pharm.
4 minutes
Prescribing cascades present a real challenge for all healthcare professionals, one which you likely tackle in your daily practice. You are undoubtedly familiar with the following scenario.
- A patient reports an unpleasant symptom, prompting a prescription for medication.
- However, the root cause of the symptom may be another medication that could have been discontinued or substituted, and unfortunately, the relationship between cause and effect was not noted.
- Consequently, the patient begins another course of medication, leading in turn to additional side effects.
We are now caught in a downward spiral from which it can be difficult to recover!
This kind of situation can have severe repercussions, including hospitalization, particularly for the most vulnerable patients. Fortunately, pharmacists can assume a pivotal role in optimizing patient therapy by adeptly detecting, resolving, and ideally preventing prescribing cascades.
Let's explore together some strategies to steer clear of these pitfalls!
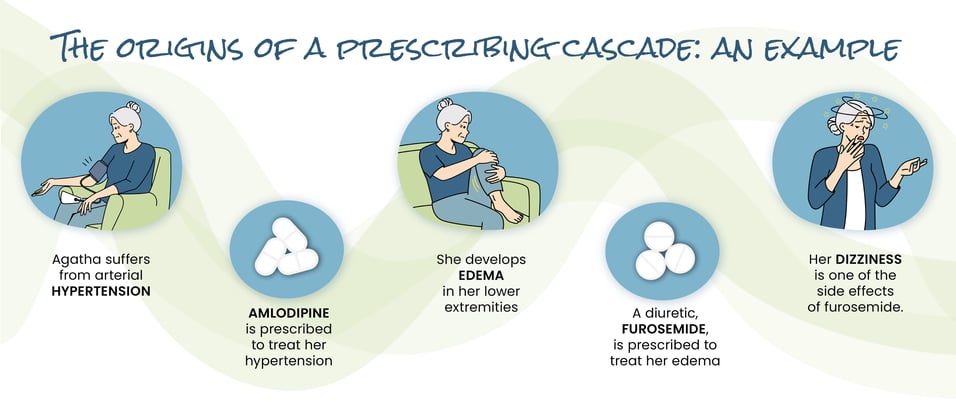
But First, Let’s Define a Prescribing Cascade
A prescribing cascade occurs when an adverse reaction to a medication is wrongly interpreted as indicative of a new pathology, leading to the prescription of additional medication.
This subsequent treatment has the potential to exacerbate the initial adverse reaction or introduce new side effects of its own.
Consequently, there is a risk of perpetuating a cycle in which medications are continually added to address the emergence of new side effects, rather than questioning from the onset whether the initial treatment was appropriate.
Below is an example.
Typical Situations You Might Come Across in Your Pharmacy Practice
-
Anticholinergics and Confusion in the Elderly. Confusion caused by an elevated anticholinergic load may be misinterpreted as a symptom of a neurocognitive disorder. This may in turn lead to the prescription of a cholinesterase inhibitor or even of an antipsychotic.
-
Antidepressants and Insomnia. A number of antidepressants can interfere with sleep, which in turn might be misinterpreted as a symptom of inadequate relief from depression. As a result, we may increase the dose of antidepressant or add a prescription for sleeping pills.
-
Calcium Channel Blockers and Edema. These antihypertensives can lead to edema of the lower limbs, which we will often tend to manage by adding a diuretic.
-
ACE Inhibitors and Cough. Up to a third of patients taking an angiotensin-converting enzyme inhibitor will eventually experience a persistent dry cough. They may be tempted to use a cough syrup on a regular basis, when in fact, the best solution would be to change their antihypertensive agent.
-
Thiazide Diuretics and Gout. Because they increase uric acid levels in the blood, these diuretics can provoke a gout flare-up. This may prompt the introduction of a treatment for gout, or in some cases of a prophylactic treatment.
-
NSAIDs and Hypertension. Prolonged use of a non-steroidal anti-inflammatory medication increases blood pressure; we therefore generally increase the dose of the current antihypertensive medication or add a second one.
-
Pregabalin, Gabapentin and Edema. These anticonvulsants, which are often used to treat neuropathic pain, are known to cause peripheral edema. To counteract this side effect, a diuretic is usually prescribed, whereas it would have been preferable to reduce the dose or use a different compound.
A prescribing cascade can be relatively simple for a diligent pharmacist to identify and resolve. For example, a bisphosphonate causes dyspepsia, therefore a PPI is prescribed. An antihypertensive drug causes dizziness, so betahistine is added.
But now, for an added level of difficulty: a benzodiazepine causes memory problems. A visit to the doctor then leads to a cognitive assessment, after which a cholinesterase inhibitor is prescribed. The latter causes nausea and urinary incontinence, for which dimenhydrinate and fesoterodine are prescribed. A few weeks later, the patient is admitted to the hospital for repeated falls and confusion.
Phew! How could we avoid the situation from reaching that point?
Recognizing a Prescribing Cascade
As time goes by and as the number of interventions grows, it becomes increasingly difficult to know whether a medication was actually intended to treat a medical problem or whether it was prescribed to counter side effects.
By being familiar with their medication history, asking them questions regularly, and considering the sequence of medication changes and the onset of their symptoms, you can simplify your work and improve the well-being of the people under your care.
Questions You Should Ask Yourself:
- Could the symptom reported by the patient be a side effect of a medication?
- Am I considering adding a medication to treat this symptom?
If you answer yes to either of these two questions:
- Can I replace the medication with a safer one, or can I reduce the dose to avoid adding a second medication?
- Does my patient really need the medication, or can it be stopped?
Preventing Prescribing Cascades
As you know, it is always much easier to prevent than to cure. The following are a few tips aimed at helping you avoid the pitfalls of prescribing cascades.
- By starting with a low dose and by gradually increasing it to reduce the risk of adverse reactions when prescribing a new medication, especially in frail, elderly patients.
- By considering, until proven otherwise, the onset of a new symptom to be an adverse reaction, especially if you have recently started a new medication therapy or if you have increased the dosage.
- By questioning your patient about the occurrence of new side effects after a dosage adjustment or the following addition of a new medication.
- By providing a plain-language information sheet on the new medication's most common side effects.
- By prescribing a new medication to counter the side effect of another only after having evaluated all the available options and checking that the benefits of continuing with the first medication outweigh the risks of adding the second.
Let's Steer Clear of These Pitfalls!
As we have seen, prescribing cascades can unfortunately easily go undetected in a patient's daily routine, and lead to potentially serious side effects, which can in turn require hospitalization. These events contribute to the polypharmacy phenomenon mainly by increasing the improper usage of specific medications. It ends up having costly consequences for both individuals and society.
As pharmacists, we can play a crucial role in detecting and managing prescribing cascades. We may not be able to completely eliminate them, but whether by identifying common patterns, thoroughly analyzing medication profiles, or asking relevant questions, we can mitigate their occurrence, thereby enhancing the quality of care we deliver to our patients.
Are you up for the challenge?
References
- Mallet, L. La cascade médicamenteuse : comment la prévenir, la détecter et résoudre les problèmes qu’elle engendre. Pharmactuel 2016 ; 49 (2) : 136-139.
- Sternberg SA et coll. Cascade médicamenteuse chez la personne âgée. CMAJ février 2021 ; 193 : E215.
- Kalisch, L. M., Caughey, G. E., Roughead, E. E., & Gilbert, A. L. (2021). The Prescribing Cascade. Australian Prescriber, 34(6), 162–166.
- Rochon, PA , Gurwitz, JH. Optimising medication treatment for elderly people: the prescribing cascade. BMJ Vol 315 (25) octobre 1997.
Barbara St-Pierre, B.Pharm.
Pharmacist, Content Team
DISCLAIMER
This blog is intended for information purposes only. The views and opinions expressed are solely those of the original authors and contributors, and do not necessarily reflect, in whole or in part, those of Vigilance Santé. Vigilance Santé makes no warranty as to the accuracy, comprehensiveness or correctness of the information contained in this blog. The information presented in this blog is in no way a substitute for professional medical advice, diagnosis, or treatment, or for the skills and expertise of a health professional. Neither Vigilance Santé (nor its shareholders, officers, directors, executives, employees, collaborators, subcontractors, and distributors) nor the authors may under any circumstances be held liable for any loss or damage directly or indirectly related to the content of this blog or its use.
