Six tips to help your breastfeeding patients with low milk supply
2024-04-15
|Annik Beauclair, B.Pharm.
4 minutes
As a pharmacist, you've probably been asked to dispense a medication used as a galactagogue to a breastfeeding patient before. A few questions likely ran through your mind:
- What could be causing this person to experience low milk supply?
- What advice can I give aside from the guidelines for the medication?
- Is there anything the patient should avoid or tips they could try?
Breastfeeding support beyond medication
Given our role as health care professionals, we know that breastfeeding benefits both the child and the person who is breastfeeding.
Moreover, we must remember that this is true even when breastfeeding is not exclusive, whether due to lack of breast milk or other reasons. The benefits are proportional to the quantity of milk received and the duration of breastfeeding.
Insufficient milk supply, be it real or perceived, is often reported as one of the causes of discontinued breastfeeding, making it all the more crucial to be proactive when problems arise.
Real vs. perceived lack of breast milk
In a situation like the one described above, your first step should be to make sure that the patient actually has an insufficient milk supply.
There are a number of misleading factors that can cause a person to underestimate how much breast milk they’re really producing. For example, the amount expressed using a breast pump is not a reliable indicator; neither is how soft or full the breasts feel. Often, the issue isn't milk supply, but rather the transfer of milk from breast to baby.
As part of this step, consider asking whether the individual has spoken to a qualified professional, such as a breastfeeding specialist (e.g., an IBCLC). If not, it's a good idea to refer them to a resource that will provide the necessary support.
From colostrum to mature milk
Different factors can lead to low milk supply depending on how long it has been since childbirth. By examining the physiology of breastfeeding, we can get to the root of certain problems and find solutions.
Before pregnancy
- The mammary gland prepares for the potential need to produce milk.
- Trauma to the breasts at this time, or insufficient development during puberty due to hormonal problems, could explain insufficient milk production in the postpartum period.
During pregnancy
- The gland develops and colostrum is produced.
- This is stage I lactogenesis. Colostrum is the first milk the body produces, making it the first milk a newborn gets when they start breastfeeding.
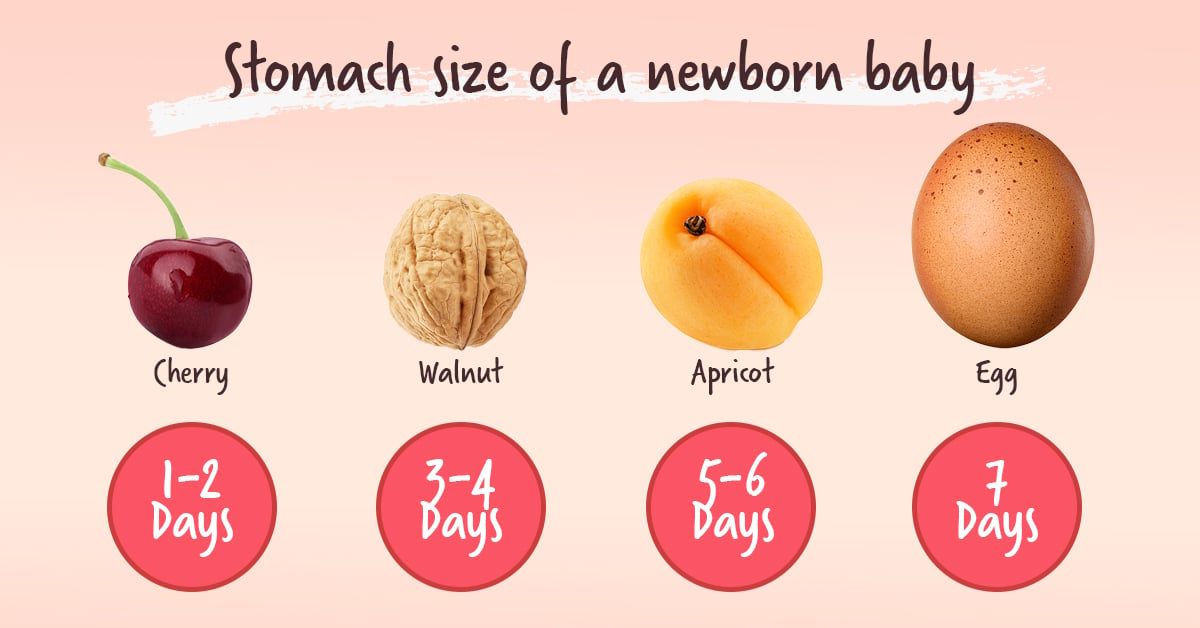
📷 A picture is worth a thousand words
According to the Government of Canada document Ten Valuable Tips for Successful Breastfeeding and the Ministère de la Santé et des Services sociaux du Québec's Fact Sheet For Nursing Mothers, a newborn's stomach in their first two days out of the womb is approximately the size of a cherry. That's why the small amount of colostrum that the breasts produce is enough to meet an infant's needs for the first few days.
During childbirth
- The sudden drop in progesterone and other inhibitory hormones triggers stage II lactogenesis, which is signalled by increased milk production.
- This will occur whether or not breastfeeding is planned as the mammary gland begins to secrete an abundant volume of milk. Certain factors can delay or hinder the onset of this stage of lactogenesis, including delivery by C-section, a retained placenta, and type 1 diabetes.
- Note that up to this point, breast milk supply is controlled by endocrine hormones.
After childbirth
- Once the baby is born, milk production will regulate based on demand.
- The more milk is removed from the breast, the more the body will produce. The breast is never empty. For this reason, maintaining optimal milk production requires effective stimulation and milk extraction.
- This phase, known as stage III lactogenesis, is controlled by both endocrine and autocrine hormones. A milk protein called the feedback inhibitor of lactation (FIL) has an inhibitory effect on lactogenic cells. If milk remains in the breast, FIL will slow down milk production. Indeed, frequently plugged ducts are an example of something that can cause decreased milk production.
We can now see why the main cause of low breast milk supply is poor milk extraction.
It's clear that even with the help of a galactagogue, milk production will not increase and may continue to decline unless the milk is frequently and regularly extracted.
Advice from a pharmacist
The table below contains suggested tips and reminders you can offer patients when filling a galactagogue prescription or during consultations for lack of breast milk.
As a pharmacist, I always suggest to my peers working in community pharmacies that they have on hand a list of references of local people trained in breastfeeding to offer to parents who seek their help. This makes it much easier to offer advice. Here are a few examples: IBCLCs, community organizations, midwives
| Nurse frequently and regularly. |
To maintain an optimal rate of milk production, it's essential to stimulate the breast and extract the milk frequently and effectively. The rule of thumb is a minimum of 8 feedings every 24 hours. Night feedings are also very important. |
| Make sure to breastfeed properly. |
Among other things, this means ensuring baby gets a good latch and that milk transfer is adequate. We can help parents breastfeed successfully by doing the following:
|
| Avoid non-nutritive sucking (pacifiers) and bottle-feeding. |
This advice is based on the fact that babies can only learn to breastfeed by breastfeeding. Consequently, if a baby requires supplemental feeding, you can start by suggesting the use of a lactation aid. |
| Opt for breast milk if supplemental feeding is required. |
Remember that oftentimes, the supply of breast milk is sufficient, but the baby isn't able to extract it. In addition, if a supplement is needed, breast milk expressed manually or with a breast pump should take precedence. Learn more about the medical indications for replacing or supplementing breast milk here. |
| Use a hospital-grade double breast pump. |
Designed to pump both breasts at once, double breast pumps maximize and accelerate milk expression. It's possible to rent hospital-grade units, which are generally more powerful than other electric models on the market. |
| Use the right-size breast pump flange. |
The flange is the funnel-shaped part of the breast pump that is placed over the nipple and areola. In order for pumping to be as comfortable and efficient as possible, it's essential to use the correct flange size. Some breast pump manufacturers sell flanges in different sizes that are compatible with their devices. For a flange sizing guide that's available in multiple languages, click here. |
If you use RxVigilance, you'll be pleased to know that the tool offers not only monographs on drugs to stimulate milk production, but also information for professionals and leaflets for breastfeeding parents, such as a health leaflet on breastfeeding and advice about contraception during this period.
Let's summarize
When counseling breastfeeding patients, there are two things we need to remember:
- Feeding the baby, and;
- Maintaining milk production.
I hope that the recommendations I've offered in this article help you enhance your clinical services, spark ideas for more holistic solutions, and encourage you to reach out to qualified external resources.
By establishing a better continuum of services for breastfeeding individuals while adopting a constructive approach, we can support them throughout their journey.
Many satiated babies will have you to thank!
Annik Beauclair, B.Pharm.
Pharmacist, content team
DISCLAIMER
This blog is intended for information purposes only. The views and opinions expressed are solely those of the original authors and contributors, and do not necessarily reflect, in whole or in part, those of Vigilance Santé. Vigilance Santé makes no warranty as to the accuracy, comprehensiveness or correctness of the information contained in this blog. The information presented in this blog is in no way a substitute for professional medical advice, diagnosis, or treatment, or for the skills and expertise of a health professional. Neither Vigilance Santé (nor its shareholders, officers, directors, executives, employees, collaborators, subcontractors, and distributors) nor the authors may under any circumstances be held liable for any loss or damage directly or indirectly related to the content of this blog or its use.
